Health
A Prospective Study On Hyponatremia In Traumatic Brain Injury
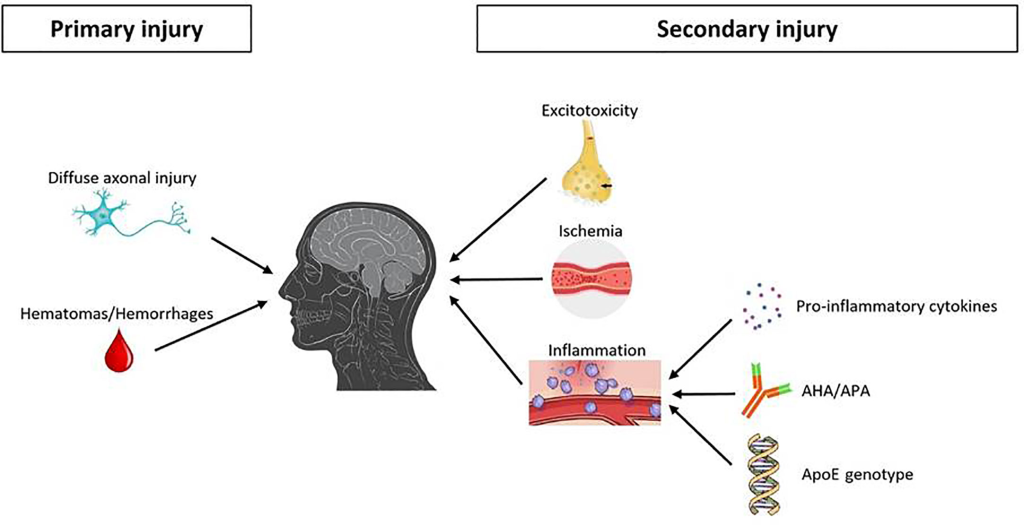
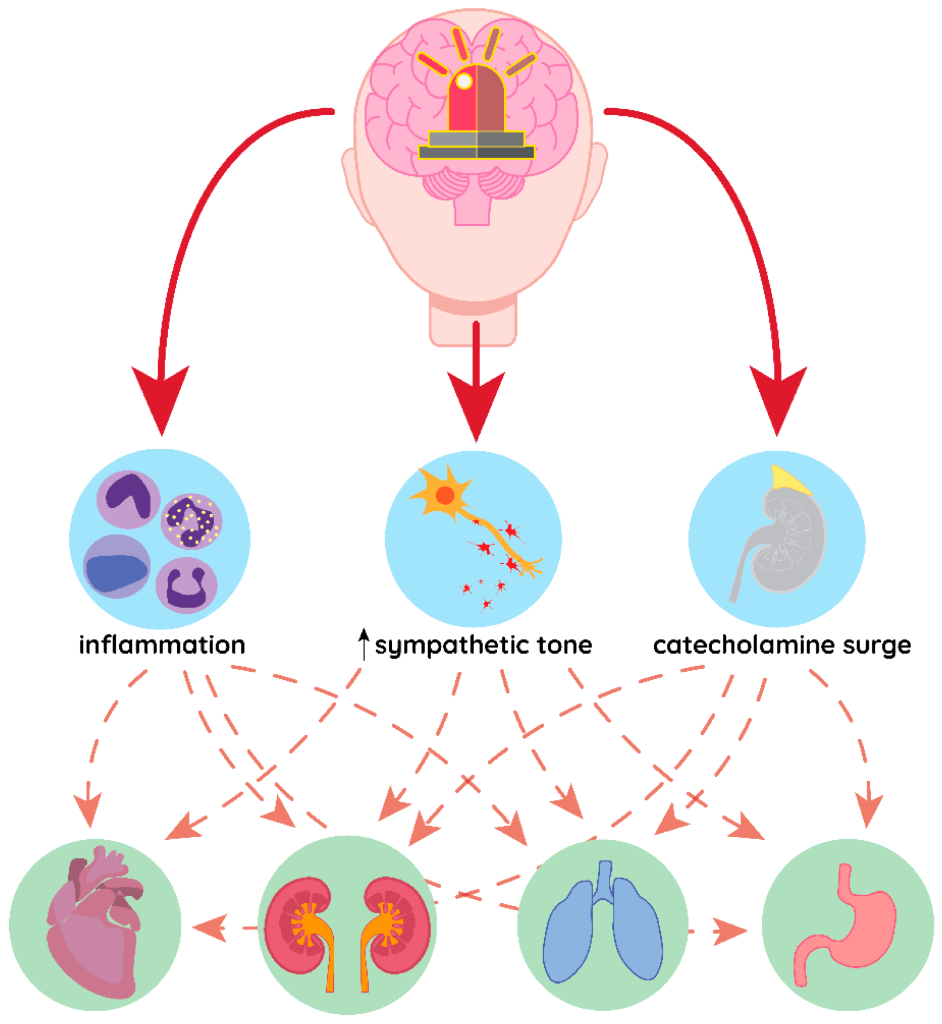
Hyponatremia is the most common electrolyte imbalance observe in traumatic brain injury (TBI). It affects 15-20% of TBI patients, with the onset occurring in the first 48 hours after the injury. The high incidence of hyponatremia in TBI is related to the disruption of the normal hypothalamic-pituitary-adrenal axis. The consequent release of antidiuretic hormone (ADH). Hyponatremia is associate with worse outcomes in TBI patients, including increase mortality. Treatment of TBI-induced hyponatremia involves careful monitoring of sodium levels, rehydration, and correction of electrolyte abnormalities if present. It is essential to provide timely.
What Does Hyponatremia Mean?
Hyponatremia, can be defined as a serum sodium concentration of below 135 mEq/L, is the most common electrolyte abnormality observe in traumatic brain injury (TBI). This electrolyte imbalance is also an independent predictor of poor neurological outcomes for those with TBI. The report incidence of hyponatremia in literature reports has been found to vary greatly. There is still difficulty in accurately predicting the risk of this electrolyte abnormality in TBI patients. Research has shown that a number of factors, such as the severity of TBI, the presence of other physiological abnormalities. The use of certain medications, can increase the risk of hyponatremia in TBI patients.
We frequently encounter hyponatremia in our practice, and as such, we decided to review data from our center to gain a better understanding of the incidence of hyponatremia. The results of our management strategies, and to formulate evidence-based, simple guidelines for the correction of hyponatremia in traumatic brain injury (TBI) patients. Our analysis focused on the impact of hyponatremia and the effectiveness of our management strategies on mortality, morbidity, and complications related to TBI. We also sought to assess the risk factors associated with hyponatremia in TBI. Consider the implications of this condition on patient outcomes. Our findings and the resulting guidelines we propose could be important for developing.
Is Hyponatremia Common In Patients?
Hyponatremia is an electrolyte imbalance that is commonly observe in patients with traumatic brain injury (TBI). This study aims to determine the incidence of hyponatremia in TBI patients. Its associated etiology, biochemical confirmation, and possible correlations with initial Glasgow Coma Scale (GCS) score and computed tomography (CT) abnormalities. Previous studies have demonstrate that the presence of hyponatremia in TBI patients is associate with poor outcomes. Making it an important factor for medical practitioners to take into consideration when assessing and treating these patients. The current study will seek to further understand the role of hyponatremia in TBI patients by analyzing its incidence, etiology, biochemical confirmation.
Observational Analytical Study On Hyponatremia:
This prospective observational analytical study was conduct from January 2015 to December 2015 in order to gain insight into a particular phenomenon. The study collected data from a variety of sources and utilized a range of analytical methods to draw valid conclusions. The data collected was analyze in a systematic and comprehensive manner to draw valid inferences and conclusions. The results of the study were then use to make inform decisions and recommendations on the matter. The findings of the study were publish in an academic journal and share with stakeholders. The study has been widely cited and has been of great value in understanding the phenomenon in question.
Patients Of Traumatic Brain Injury
Mild and moderate traumatic brain injury (TBI) patients aged between 13 and 65 years, with no comorbid conditions, were include in the study. Patients were monitor for hyponatremia, and the etiology was determine through a comprehensive investigation protocol. This involved a comprehensive physical examination, an assessment of the patient’s medical history, and laboratory investigations. The results of these tests were compare to the patient’s clinical presentation, and any discrepancies were investigate further. Through this process, the etiology of hyponatremia was successfully identify in each of the patients.
Hyponatremia Was Defined As Serum Sodium:
A retrospective analysis was conduct on 1,500 consecutively admit patients with traumatic brain injury (TBI). It using an electronic records system and radiographic review. The purpose of the analysis was to assess patient-related factors that may contribute to the occurrence of traumatic brain injury. The subsequent treatment of individuals who have sustained a TBI. All data was gather and statistically evaluate to identify patterns and trends in the data set. This study was conduct to further our understanding of the epidemiology of TBI. As well as to identify any possible factors related to the successful management of TBI in the clinical setting. Through this analysis, we hope to identify opportunities to improve the caring quality for patients with TBI.
Hyponatremia is a medical condition characterize by abnormally low levels of sodium in the blood. It usually defined as serum sodium concentration below 135 mEq/L. Natriuresis is a medical term for an increased rate of excretion of sodium in the urine. It usually defined as a urine spot sodium concentration of more than 40 mEq/L. To evaluate the incidence of traumatic brain injury (TBI), its management, and the effect of fludrocortisone. A study was conduct on a group of individuals with hyponatremia and natriuresis. The results of the study demonstrated that fludrocortisone was an effective treatment for TBI in individuals with hyponatrem.
Methods:
All patients aged 20 years and older presenting with TBI of any severity. As well as mild TBI cases presenting with CT abnormality, were include in this study. The severity of the TBI was assess using internationally accepted criteria. Including Glasgow Coma Scale scores, duration of post-traumatic amnesia, and presence of Skull fracture or intracranial haemorrhage. Furthermore, the CT scan results were analyze to determine the presence of any abnormality. Daily sodium levels were closely monitor in all patients for 14 days.
In order to evaluate volume status, central venous pressure (CVP) was also measure. Furthermore, fractional excretion of uric acid (FEUA) was calculate in all patients with hyponatremia before and after its correction. In order to gain an accurate understanding of its impact on the patients’ health. The results of these tests allowed us to obtain valuable insight into the effects of sodium levels on the patients’ overall health and wellbeing.
Incidence Of Hyponatremia
Our study revealed an incidence of 13.2% for hyponatremia. We found that early therapy with fludrocortisone had a significant effect on reducing hospital stay duration (P < 0.05). We found that, compared to the control group, patients treated with fludrocortisone had a significantly shorter hospital stay (mean difference of 4.5 days). Analyses revealed that early treatment with fludrocortisone was associate with a mean reduction of hospital stay of 4.5 days.
While further research is need to confirm these findings, our study provides evidence for the efficacy of early treatment. treatments include fludrocortisone in reducing the duration of hospital stay for patients with hyponatrem. A total of 153 patients were include in the study, of which 33 (21.6%) were find to be suffering from hyponatremia. The present study aimed to evaluate the incidence of hyponatremia in patients of a certain population. The results suggest that hyponatremia is a relatively common phenomenon. Further research is need to investigate the underlying causes and potential treatments for this condition.
Most Commonly Identified Abnormality:
Traumatic subarachnoid hemorrhage was the most commonly identify abnormality on admission compute tomographic scans among patients who present with hyponatremia. This finding was observe in a retrospective study involving a cohort of patients at a tertiary care center. Who had been hospitalize for hyponatremia-related causes. The results of the study indicated that traumatic subarachnoid hemorrhage, which is a bleeding of the layer of cerebrospinal fluid. Surrounds the brain, was the most commonly identify abnormality for these patients. Furthermore, the study found that the presence of this abnormality was associate with increase mortality rates for hyponatremia-related causes.
Results:
Cerebral salt wasting syndrome found to be more common than the syndrome of inappropriate secretion of antidiuretic hormone (SIADH) in a recent study. Specifically, incidence was higher in patients with lower Glasgow coma scale scores (p = 0.001). In patients with parenchymal contusions (p = 0.008). It is important to note that the two syndromes share many of the same symptoms, such as hyponatremia, hypotension and hypovolemia. Makes it difficult to differentiate between the two. Further research is necessary to more accurately identify which syndrome is present in a given patient.
The incidence of hyponatremia found to have a strong positive correlation with the Marshal computed tomography (CT) score (p = 0.013). There was no significant difference between genders or age groups in terms of incidence. Furthermore, patients with hyponatremia had a significantly longer duration of stay in both the intensive care unit (p < 0.001) and hospital (p < 0.001). These results suggest that the severity of hyponatremia, as measured by the Marshal CT, is a strong predictor of time spent in the ICU and hospital.
Outcomes:
At the time of hospital discharge, patients with hyponatremia had significantly worse outcomes. When compared to those without hyponatremia (p = 0.002). However, no significant difference in outcomes was observed between the two groups at the 3-month follow-up (p = 0.087). The results of this study suggest that while the presence of hyponatremia may have a negative impact on outcomes at hospital discharge. The effects may not persist beyond that time frame. Further research should be undertaken to examine the long-term impact of hyponatremia on patient outcomes.
Final Report:
In a study of 40 consecutive patients, 33 remained for analysis. Hyponatremia was seen in 9 (27.2%) of those patients, 6 of whom developed it within the first week of observation. The mean duration of hyponatremia was 1.78 days. Further, 5 patients were observed to have an elevated CVP, which is consistent with the syndrome of inappropriate antidiuretic hormone (SIADH). These findings suggest that hyponatremia is a common symptom in this population and that SIADH could be a contributing factor. Further studies are needed to analyze the exact cause of hyponatremia and the role SIADH plays in the development of this condition.
Measurement of FEUA did not show a consistent pattern that would suggest a biochemical distinction between mild, moderate, and severe TBI. Among hyponatremic patients, the distribution of mild, moderate, and severe TBI was equal at 33.3% each. Furthermore, a positive correlation was observed between Rotterdam CT scores and incidence of hyponatremia (r = 0.983, P = 0.017), suggesting that the severity of TBI is an important factor in the development of hyponatremia. Specifically, hyponatremia was seen in Rotterdam CT scores I to IV with increasing incidence. These findings point to the importance of monitoring the electrolyte levels of patients.
Hyponatremia Due To SIADH:
Hyponatremia due to Syndrome of Inappropriate Antidiuretic Hormone (SIADH) secretion is more commonly seen in traumatic brain injury (TBI) patients, as compared to other etiologies. Although fractional excretion of urea (FEUA) measurement has been used to differentiate between SIADH and cerebral salt wasting syndrome (CSWS), its accuracy has not been consistent enough to make a reliable distinction. A more reliable predictor of hyponatremia in the setting of TBI is computed tomography (CT) scoring of injury severity. Initial Glasgow Coma Scale (GCS) scores have demonstrated less predictability for hyponatremia in this population.
Early Initiation Of Fludrocortisone:
Early initiation of fludrocortisone treatment has been found to be beneficial in the setting of hyponatremia with natriuresis, as this helps to reduce the duration of the patient’s hospital stay. Studies have demonstrated that this approach can help to reduce the patient’s amount of time spent in the hospital, as well as any associated medical costs. Fludrocortisone is thought to act by increasing free water clearance, thus allowing for the excretion of excess sodium and the restoration of serum osmolality. This treatment has been found to be especially useful in the elderly population, who are more prone to developing hyponatremia due to underlying conditions such as hypothalamic dysfunction, and heart failure.
This protocol is likely to be a more suitable option in a tropical country, where fluid restriction may be contraindicated due to the climate. Furthermore, it eliminates the need to differentiate between the etiology of SIADH (syndrome of inappropriate antidiuretic hormone secretion) and CSW (cerebral salt wasting), two conditions which may present with similar symptoms. This protocol is preferable for its ability to provide a more comprehensive approach in managing the associated symptoms of these disorders, allowing for a tailored and individualized treatment plan according to the patient’s needs. Additionally, it may help to reduce the risk of misdiagnosis of these disorders.
Conclusion:
Hyponatremia is a very common electrolyte imbalance among patients with traumatic brain injury (TBI). The Marshall CT grading and initial Glasgow coma scale score have been found to have a strong correlation with the risk of developing hyponatremia. Therefore, aggressive sodium monitoring may be necessary in order to detect any increases in the risk of hyponatremia, especially in cases of parenchymal contusions. Such monitoring should be conducted regularly in order to identify any signs of hyponatremia in the patient in a timely manner, allowing for appropriate interventions to be implemented. Moreover, medical professionals must take into account the patient’s age, as well as their neurological and medical history.
Frequently Asked Questions
Why brain injury causes hyponatremia?
Hyponatremia usually indicates underlying disorders that disrupt fluid homeostasis. In most patients with TBI, hyponatremia is a feature of the syndrome of inappropriate antidiuretic hormone (SIADH) secretion due to pituitary dysfunction after head injury.
What causes hyponatremia in trauma?
The most common causes of hyponatremia after traumatic brain injury (TBI) are syndrome of inappropriate antidiuretic hormone secretion (SIADH) and cerebral salt-wasting syndrome, while post-traumatic hypopituitarism is a rare cause of severe hyponatremia.
Hyponatremia commonly occurs in patients with aneurysmal subarachnoid hemorrhage. Two mechanisms have been proposed as causes: syndrome of inappropriate anti-diuretic hormone and cerebral salt wasting.